Abstract
Background:
Inferior vena cava (IVC) filters are commonly placed in patients with contraindications to anticoagulation including bleeding concurrent with venous thromboembolism (VTE). Retrievable IVC filters have been preferred over permanent filters for their flexibility to be removed once anticoagulation can be resumed. Published reports show that the retrieval rate of the filters is around 34%. Non-retrieved filters can result in significant complications such as filter migration, embolization, filter fracture, vena cava thrombosis, and IVC perforation.
Objective:
The primary objective of this study is to assess IVC filter insertion indications, retrieval rate and factors prohibiting timely retrieval.
Methods:
A retrospective chart review was conducted on patients with a history of IVC filter placement and/or removal between January 2012 and January 2017. Data collected included demographics, indications for filter placement, referring and placement services and the reasons for non-retrieval.
Results:
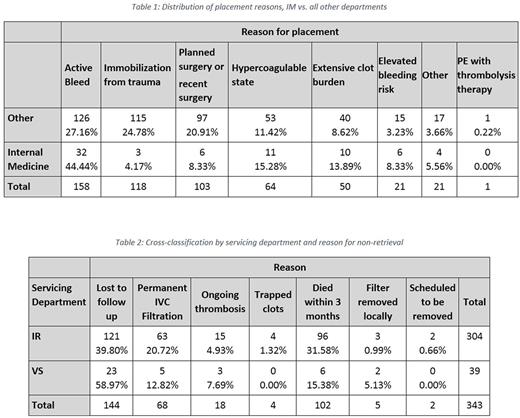
A total of 573 patients were identified of which 343 patients had IVC filters inserted without retrieval, 200 patients had placement followed by retrieval and 30 patients who had retrieval alone. Reasons for placement included VTE with active bleed in 29.48%, trauma, surgery, or immobilization in 22.01%, VTE with planned surgery in 19.22%, history of VTE with planned surgery in 11.94%, and extensive clot burden in 9.33%, VTE with elevated bleeding risk in 3.92%, PE with thrombolysis therapy in 0.19%, and other in 3.92% of patients. Internal medicine had ordered IVC filters in 44.44% of patients compared to 27.16% in surgical services with (p-value of 0.0028). This indicates that a significantly greater proportion of IVC filters were placed due to VTE with active bleeding in internal medicine as opposed to all other departments. In addition, Internal medicine ordered IVC filters for immobilization from trauma in 4.23% of patients compared to 24.73% by other departments (p-value <0.0001), indicating that other departments order IVC filters for immobilization or bleeding from trauma at a significantly higher rate than does internal medicine.
For those 343 patients who had IVC filters placed but not retrieved, reasons for non retrieval by Interventional radiology(IR) included lost to follow up in 39.80% compared to 58.97% in vascular surgery, decided to use as permanent IVC filter in 20.72% in IR compared to 12.82% in vascular surgery, ongoing thrombosis in 4.93% in IR compared to 7.69% in vascular surgery, trapped clots in 1.32% in IR compared to 0% in vascular surgery, died within 3 months in 31.58% in IR compared to 15.38% in vascular surgery, filter removed locally in 0.99% in IR compared to 5.13% in vascular surgery, and scheduled to be removed in 0.66% in IR compared to 0% vascular surgery.
To further investigate the rates of patients that were "lost to follow up" we dichotomized the reasons into "lost to follow up" in comparison to all other reasons. This showed that the reason for non-retrieval was lost to follow up in 39.80% compared to 58.97% of patients in vascular surgery (p-value 0.0224). This indicates that the proportion of patients that were "lost to follow up" in vascular surgery is significantly higher than in interventional radiology.
Conclusion:
Only one-third of IVC filters were ordered in compliance to current evidence based guidelines. There was also a significantly greater proportion of "lost to follow up" patients in vascular surgery compared to interventional radiology, indicating room for improvement regarding patient follow up. To improve the appropriateness of IVC filter insertion and overall retrieval rate, we plan to implement best practice alerts and institutional guidelines along with hematology referral upon patient discharge to aid in timely retrieval. We plan to reevaluate our practice in 6 months following the implementation of these guidelines.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal